Patient Education
At Amery Vein & Wellness Center, we're committed to providing the highest standard of professional care and personalized patient experience that you deserve.
Restore the Health and Beauty of Your Legs
The most common venous conditions are spider and varicose veins, however both can lead to much more serious conditions, including blood clots that form in the superficial and deep veins (aka Superficial and Deep Vein Thrombosis). Spider and Varicose veins can also be a sign of Chronic Venous Insufficiency. Vein disorders are not always visible; diagnostic techniques are important tools in determining the cause and severity of the problem. Contact Amery Vein and Wellness Center to see if you qualify for a Free Vein Health Screening.
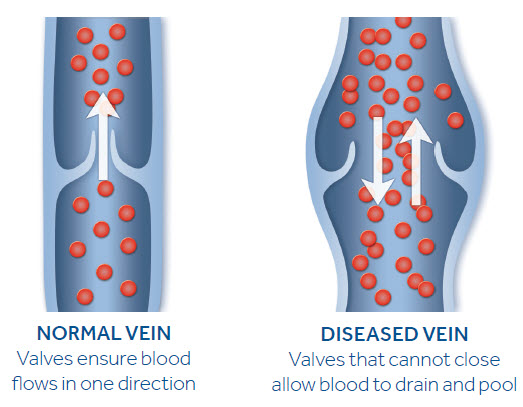
If you’re over 40, you probably see them; those little purple veins that suddenly seem to appear on your legs. Veins are the soft, thin-walled tubes that return blood from the arms and legs to the heart. Because veins work against the force of gravity, they have valves that allow forward blood flow, but not reverse. Your legs and arms have two major types of veins: superficial and deep. The superficial veins are near the surface of the skin and are often visible. The deep veins are located near the bones and are surrounded by muscle. Connecting the deep and superficial veins is a third type of vein, the perforator vein. Contraction (squeezing) of the muscles in the arms and legs with exercise helps blood flow in the veins. Varicose veins are enlarged, bulging superficial veins that can be felt beneath the skin, generally larger than 3-mm in diameter. They are usually located on the inside of the calf or thigh and develop due to weakness of the vein wall and loss of valve function. Under the pressure of gravity, they continue to enlarge, and in the course of time, they may become elongated, twisted, pouched and thickened. Spider veins or telangiectasia are tiny dilated, veins, usually less than 1-mm in diameter, located at the surface skin layers. Veins larger than the spider veins, but still under 3-mm are called reticular veins.
To understand the causes of venous disorders, you have to start with the circulatory system. Our circulatory system is made up of two separate parts: arteries that take the blood from the heart to all the tissues in our bodies and veins that return the blood back to our heart. The arteries benefit from gravity, which pulls the blood downward from our heart, whereas the veins have to generate their own pumping action to resist gravity and move the blood back up to our heart. To move the blood in this way, our veins are arranged in two layers: deep veins that run vertically within our muscles and superficial veins that are arranged as a network of thousands of vessels. When the veins are unable to pump blood properly, blood begins to pool in our veins instead of moving upward toward our heart. This pooling is what leads to the appearance of spider and varicose veins as well as the more serious symptoms for leg pain, leg swelling, and blood clotting.
There are several risk factors that contribute to vein disease:
Aging is one of the most important risk factors. Small venous problems often progress into large ones over time. A decrease in the body’s production of collagen, a breakdown of the elastic material in vein walls causes them to breakdown and stretch over time, which ultimately results in bulging veins, more visible veins, and swelling in the veins.
Genetics is also a significant risk factor. Vein disorders run in families, and if you have a family member with spider or varicose veins, you are more likely to develop them yourself.
Ethnicity also plays a role in the development of venous disorders. Research has found that Caucasians have a higher incidence of varicose veins than people of Hispanic, African American, and Asian descent.
Mobility can be an important treatment method as well as a risk factor. Sitting, lying, and particularly standing for long periods of time hinders the ability of the leg muscles to pump blood, slowing down the blood flow.
The severity of vein diseases can range from cosmetic to life-threatening, so it’s important to consult a vein care specialist if you think you have a venous disorder or are considering different treatment options. A vein care specialist will be able to evaluate the severity of your condition and recommend different treatment options.
Varicose veins may be entirely symptom-free and cause no health problems. Treatment in such cases is often for cosmetic purposes. When symptomatic, you may experience the following:
• Ankle and leg swelling
• Heaviness or tension
• Aching in the legs
• Restless legs
• Night cramps in the legs
• Itching in the legs
• Skin pigmentation (brownish)
Varicose veins are more often symptomatic in women than in men. Itching is perhaps the most consistent symptom of varicose veins in men. Women most often complain of leg heaviness, tension and aching.
The most important factors leading to the development of varicose veins include:
• Heredity
• Prolonged standing
• Increasing age
• Heavy lifting
• Prior superficial or deep vein clots
• Female gender
• Multiple pregnancies
Less physical activity, a higher blood pressure and obesity have also been linked with the presence of varicose veins in females.
Typically, a Vein Health Screening contains three components: a clinical history, a physical examination, and a discussion about your treatment expectations and concerns. When seeking treatment for venous disorders, it is important to remember that vein disease is a lifelong problem that cannot be cured with a single procedure or treatment. Cosmetic reduction in visibility of spider and varicose veins is very possible, however most patients will continue to develop new spider veins throughout their lives.
Medical History
Exams
Treatment Discussion
Veins that are cosmetically unappealing or cause pain or other symptoms are prime candidates for treatment. There are two general treatment options: conservative measures, such as compression stockings and corrective measures such as sclerotherapy, radiofrequency and light source/laser treatment. In some cases, a combination of treatment methods works best. A number of factors go into determining the right treatment for you, including your desired outcomes and the severity of your condition.
Compression Stockings
Graduated compression stockings are first line of defense and a mainstay of conservative management of venous disease. Graduated compression stockings create a tight pressure around the foot and ankle that gradually decreases as it moves up the leg. This “graduated compression” promotes the normal flow of blood up the leg. Most vein specialist recommend that patients who suffer from spider veins, varicose veins, or venous insufficiency wear compression stockings. Compression stockings can also be used to supplement other forms of treatment.
Sclerotherapy
Ultrasound Guided Sclerotherapy (Echo-Sclerotherapy) is another in-office treatment alternative to surgical stripping. With this technique and based on the clinical judgment of the doctor, sclerotherapy is done with either a liquid or “foamed” sclerosant, while the doctor visually monitors the vein on an ultrasound screen. This enables treatment of veins that can’t be seen because they are below the surface of the skin and would otherwise require surgical removal. Ultrasound imaging is used to guide a needle into the abnormal vein and deliver medication to destroy the lining of the blood vessel and seal it shut. Ultrasound guided sclerotherapy is primarily used to treat large veins beneath the surface of the skin.
Radiofrequency Ablation
Endovenous Radio Frequency Ablation is a minimally invasive, in-office treatment alternative to surgical stripping of the great saphenous vein. Instead of removing the saphenous vein, it is sealed closed in place. The skin on the inside of the knee is anesthetized and a radio-frequency catheter is inserted into the damaged vein through a needle stick in the skin. The catheter delivers radiofrequency energy to the vein wall causing it to heat. As the vein warms, it collapses and seals shut.
Endovenous Laser Ablation (EVLT)
Ambulatory Phlebectomy
Ambulatory phlebectomy is a method of surgical removal of surface varicose veins. Ambulatory phlebectomy is usually performed in a doctor’s office using local anesthesia. The area surrounding the varicose vein clusters is flooded with anesthetic fluid. A needle is then used to make a puncture next to the varicose vein and a small hook is inserted into the needle hole and the varicose vein is grasped and removed. The punctures typically leave nearly imperceptible scars.
With the evaluation and treatment methods available today, spider and varicose veins can be treated in minimally invasive but effective ways that were not possible in the past. When seeking treatment for venous disorders, it is important to remember that vein disease is a lifelong problem that cannot be cured with a single procedure or treatment. Although there is no cure for venous disorders, there are many treatment options that can reduce the appearance and painful symptoms of spider veins, varicose veins, and chronic venous insufficiency. The results will depend on the treatment options chosen. But regardless of which treatment method is used, its success depends on the careful assessment and treatment by a knowledgeable vein care specialist. You are in experienced, highly qualified and compassionate care with Dr. Amery!
There are several adverse consequences of untreated varicose veins, and their severity will vary from person to person depending on their circumstances. Many people who don’t treat their varicose veins will experience continued symptoms of pain, fatigue and swelling of the legs or ankles. More advanced medical problems can include hyperpigmentation, lipodermosclerosis, venous leg ulcers, spontaneous bleeding, superficial thrombophlebitis, and a potentially life-threatening condition called deep vein thrombosis. If you’re unsure of the severity of your varicose veins, you should schedule a consultation with Dr. Amery, who will be able to determine the severity of your condition and whether treatment is necessary.
Blood that pools in the varicose veins is depleted of oxygen and nutrients. The veins also do not tolerate high pressure well and begin to allow red blood cells and fluid to leak into the tissues of the leg, which causes painful swelling. The red blood cells in the tissues cause chronic inflammation and the skin becomes dark and discolored. The medical term for the dark discoloration is hyperpigmentation.
When the skin and the fat under the skin are inflamed for years, the tissues become woody and firm. The medical term for this woody, hard tissue is lipodermosclerosis.
A condition that may occur over time, when there is chronic venous insufficiency, is a venous leg ulcer. The ulcers due to varicose veins are painful and difficult to heal. Sometimes the ulcers cannot be healed until the backward blood flow in the veins is corrected.
Another possible consequence of untreated varicose veins is spontaneous bleeding from the varicose veins. As the skin over the veins becomes thin, eventually the vein can be exposed to the outside world and be easily injured by clothing, bedding, etc. The blood loss can be significant and is painless.
Superficial thrombophlebitis (ST) is an inflammation of a vein just below the surface of the skin. The cause of inflammation is not an infection. Rather, inflammation is due to decreased blood flow through the vein, damage to the vein and blood clotting. The features of ST include redness to the skin and a firm, tender, warm vein. Localized leg pain and swelling may occur as well.
Deep vein thrombosis (DVT), unlike ST, can be associated with significant and serious medical problems. DVT is often first noticed as a “pulling” sensation in the calf of the lower leg, and it can be quite painful. Symptoms also include associated warmth, redness and swelling. The swelling often extends to above the knee.
Some patients are at higher risk for developing DVT. These include people with one or more of the following characteristics:
-
Over 60 years of age
-
Recent surgery
-
History of prior DVT
-
Prolonged immobility/paralysis
-
Malignancy
-
Blood Clotting Disorders
-
Obesity
-
Pregnancy and Postpartum
-
Infection
When a diagnosis of DVT is made, anticoagulation treatments are often started. Anticoagulation prevents progression of the blood clot, breaks up the clot and prevents the clot from traveling to the lungs. If a clot travels to the lungs it is called a “pulmonary embolus” and the outcome can be fatal.
If you’re not sure whether you need to treat your varicose veins, please call to schedule a consultation. Dr. Amery will be able to evaluate your condition and determine what kind of treatment is needed.
Do you have questions about vein treatment?
Contact us to see if you qualify for a free vein health screening. We will be happy to talk with you about your options and what to expect before, during and after treatment.
